NOTE: I want to focus the discussion on E2 even though I’m including my entire TRT protocol.
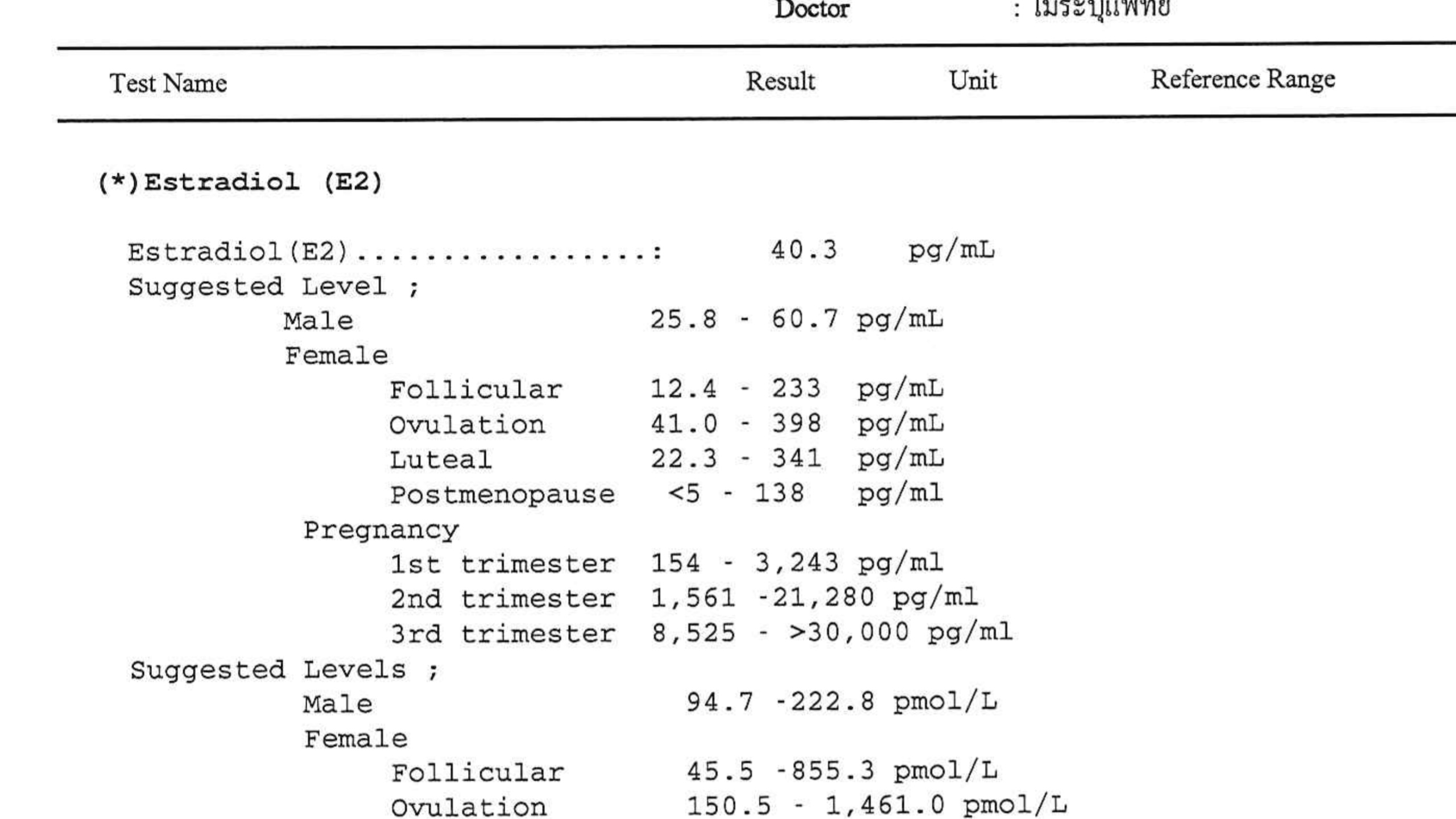
I read that the E2 reference range is 25 - 60 pg/ml. this is the reference range used by my clinic. But almost every post I read here seems to suggest this reference range is wrong…and that anything above 30 is too high.
Are there different ways of measuring E2 or is my clinic using some outdated or inaccurate reference range?
My e2 was 32 before starting any kind of therapy.
I’m 36 years old, so I tried a trial of HCG monotherapy at 500iu EOD, where my E2 went up to 46 after the first week.
I got put on an AI once a week. Eventually E2 got down to 33. after a couple more weeks.
After about 2 months on HCG mono I decided it wasn’t for me. I was moody and just felt off even though my energy levels increased. I did a final blood test before switching to TRT and my e2 was at 40.
Then I switched to TRT, and this was 5 weeks ago.
-62.5 mg testosterone 2X a week
-HCG 500IU 2X a week
-arimidex 0.125mg 2x a week.
After two weeks on this, my E2 went down to 23 pg/ml:
Total T: 1304 (lab tested only one day after injection…this was a misunderstanding, I should have waited another 2 or 3 days)
E2: 23 pg/ml (took a 0.125 arimidex pill the previous day)
And honestly…I felt better during this time…like my mood was more stable then before.
23 pg/ml is below their ref range of 25.8 to 60.7 pg/ml, so my doc told me to take the arimidex of 0.125 only once a week.
She also lowered my tesosterone dosage to 100mg /week since it was above therapeutic levels.
So since we were changing my protocol, she wanted to have another lab test done in 2 weeks…which we did and the results came at:
E2: 40 pg/ml
Total T: 1080 ng/dl
So the E2 went from 23 to 40 in 2 weeks after halfing the AI dosage. This worried me.
My doc said to continue this protocol. She thinks 40 should be where I should keep my E2.
But here’s the thing: I just felt much better during the time I tested at 23 pg/ml…my libido felt better, I had more frequent and stronger morning wood. And I could get out of bed much more easily.
So having experienced being at levels in the low 20s, low 30s, and low to mid 40s…and I can say that I think I felt best when I was in the 20s.
It’s been 2 or 2.5 weeks since I switched to 0.125 only once a week…and I feel much worse, especially in the mornings, starting about a week ago.
My doctor wants my next lab test to be in one month. But my concern is that if my e2 went from 23 to 40 in 2 weeks just after halfing my dose…I worry it will continue to go up to the 50s or 60s in a month.
So what do you think? Am I jumping to conclusions by blaming my condition on E2…could it be the exogenous testosterone at 5 weeks hasn’t stabilized yet?





 lab an reference range
lab an reference range